Advanced Primary Care Key to Reducing Health Inequities
June 14th, 2023
Robust, comprehensive primary care – a critical foundation for a more cost-effective, high-functioning health system – is equally important in helping boost health equity, a new report states.
The report, produced by the California Health Care Foundation, underscores the variety of ways in which advanced primary care can advance equity in care access and quality for underserved populations. Yet it also warns of significant barriers that continue to thwart primary care’s potential in California and nationwide.
In the face of these obstacles, employers can take steps today to strengthen primary care and reduce health care inequities. Actions can include expanding primary care locations, pushing insurers to strengthen financial support for primary care and increasing telehealth capabilities.
Unlocking Health Equity through Advanced Primary Care
Long-standing racial and economic discrimination in health and social policy has fostered pervasive health gaps for people of color. These disparities range from greater disease burdens and more mental health problems for racially minoritized populations to increased mortality and shorter life expectancies. Historically marginalized racial and ethnic groups also contend with less insurance coverage and reduced access to care.
The good news is that the key components of advanced primary care are particularly well-suited for reversing systemic health care inequities, according to the California Health Care Foundation report. Primary care’s capabilities and resulting benefits include:
- Improved access: A higher density of primary care physicians has been repeatedly linked to increased preventive services, lower avoidable morbidity and mortality and longer life expectancy among Black populations. Increasing the supply of diverse primary care doctors also helps reduce racial disparities in referral patterns and increases needed hospital care for Black Americans.
- Improved care continuity: Ongoing, individualized care provided by a single primary care clinician or practice is tied to lower mortality rates and fewer disparities in receiving recommended cancer screenings among Black and Latino populations. Interpersonal continuity with a primary care practitioner likewise enhances patient trust, which translates into better adherence to recommended preventive services, treatments and medications.
- Better coordination of care: Continuity across provider types and health care settings is shown to reduce racial and ethnic inequities in many important areas, including preventable emergency department visits and improved blood pressure control. For patients with multiple chronic conditions, coordination also lessens the burden of interacting with a fragmented and disorganized care system.
- Greater comprehensiveness: Integrating behavioral health and primary care services is considered one of the most effective ways to improve mental and physical health outcomes while eliminating inequities in care quality and access for racial and ethnic minority populations.
- Whole-person orientation: Elements of accountable, whole-person care — including clinician knowledge of a person’s overall medical history, social needs, preferences, family and cultural beliefs — improves patient self-management for chronic conditions. This is important for patients from racially and ethnically minoritized groups, who are more likely to suffer from complex comorbidities.
Advanced primary care’s power to mitigate health inequities highlights the wider benefits it can produce. Adults who regularly see a primary care physician have 33% lower health care costs and reduced odds of dying prematurely than those who see only a specialist. Every $1 increase in primary care spending produces $13 in savings.
Despite these critical advantages, primary care remains woefully under-resourced, accounting for 35% of health care visits yet only receiving 5.4% of all spending on health care in the U.S. Reimbursement for Medicaid services for low-income, at-risk populations is significantly less than Medicare and commercial rates. As a result, many young doctors burdened with student debt opt for better-paying specialties, exacerbating an already severe primary care clinician shortage.
Employers Can Take Steps to Bolster Primary Care and Advance Health Equity
Notwithstanding these challenges, employers can take steps today to accelerate advanced primary care to help reverse inequities and improve overall employee health, including:
- Increasing the overall proportion of funds dedicated to primary care. Ask your health plan what percentage of spending currently goes to primary care and work to develop incremental increases over time. To track health plan performance over time and hold plans accountable for performance, more than two dozen members of the Purchaser Business Group on Health have signed onto a first-of-its-kind tool called the Health Value Index, which creates actionable insight into a purchaser’s health plan spending and incentivizes both short- and long-term improvements in care for participating companies’ employees.
- Request data on self-identified race and ethnicity, language preference, disability status, etc.: Ask providers and plans to report their REaL (Race, Ethnicity and Language) and other data and to identify how they’re working to address health care inequities. With this data you can also begin to identify gaps in equity among your employees and families. Some easy places to start is stratifying primary care spend and use of a primary care clinician by REAL and other data to identify gaps to focus on within plan design. This work is difficult, so it could require engaging with experts to help you develop and apply a shared structural understanding of racial inequities to ensure that your team is generating accurate, helpful and actionable insights from data analysis.
- Ensuring access to telehealth that is coordinated with primary care. Telehealth has emerged as a critical tool for advancing health equity by increasing access for underserved populations. Employers should ensure that telehealth services are available for employees, as well as go one step further by working with vendors to ensure that telehealth services are coordinated with the employee’s primary care physician. When telehealth is a service provided by the primary care clinician, this coordination is already in place, however there are many third-party vendors offering telehealth services and employers should be thoughtful in terms of mitigating the risk of creating a two-tiered system that contributes to fragmentation of care.
- Adopting a holistic approach to employee health benefits. Employers should work with their plans to ensure collection and identification of social risk factors and needs that could be affecting their employee population. This would allow for holistic benefits design that could provide assistance to employees with addressing social needs that can have negative, long-term impacts on employee health.
- Ensuring adequate mental health resources. Ideally, behavioral health capabilities should be integrated with primary care to increase access and whole-person care. Setting this expectation for health plans and providers as a purchaser, as well as increasing investment into primary care to ensure these services can be funded, will help ensure these resources are prioritized and funded.
- Expanding after-hours primary care access. There are multiple models supporting after-hours care, including use of telemedicine or expanding clinic hours. Ultimately, purchasers must champion payment reform that will make these types of services possible. Much like with mental health, employers can support this conversation by also highlighting after-hours primary care access as an expectation that this is a part of critical infrastructure and including it in the purchase and payment of services.
Transforming Health Care Through Primary Care
Given advanced primary care’s unmatched ability to both address inequity and transform our health system, consensus is building around efforts to overcome longstanding financial barriers and dramatically strengthen the nation’s primary care infrastructure.
The California Health Care Foundation report, for example, calls for a new paradigm that includes programs to increase recruiting and training of primary care physicians, increased primary care spending, improved Medicaid reimbursement and expanded primary care hours and locations. Employers can play an essential role in pushing payers to invest in primary care, as well as encourage providers to use the investment to realize and extend the many benefits advanced primary care offers.
Ultimately, it is about increasing equal access to high-quality primary care for all. Having access is equity.
Special thanks to Rishi Manchanda, M.D., co-author of the CHCF report.
Employers Are Driving Innovations in Primary Care
February 24th, 2022
Employers know that primary care is essential for a healthy workforce and employees’ access to a high-value health care system. Evidence shows that improved primary care translates into healthier, happier patients and lower overall health care costs:
- U.S. adults who regularly see a primary care physician have 33% lower health care costs and 19% lower odds of dying prematurely than those who see only a specialist.
- The U.S. could save $67 billion each year if everyone used a primary care provider as their principal source of care.
- Every $1 increase in primary care spending produces $13 in savings.
Large employers are increasingly working with existing direct contracting partners and new vendors to enhance primary care, which includes the integration of behavioral health care among other things.
Four approaches reflect the ways large employers are currently working to improve primary care for their employees:
1. Developing a common set of advanced primary care standards to enable employers to speak with one voice. The development of the advanced primary care model is as much about streamlining the practice of primary care as it is about improving outcomes, enhancing the patient experience and reducing costs. Simple and consistent definitions of optimized primary care across all payer contracts would reduce, if not eliminate, the bewildering array of sometimes-conflicting value-based requirements contained in multiple payer contracts. That fact could mitigate clinician burnout by easing the administrative burden while allowing more time for the actual provision of care.
It is, therefore, essential that employers send a common signal to the market. For that reason, PBGH worked last year with members through an employer-led initiative to create a Common Purchasing Agreement. This enables employers to communicate their priorities and engage payers and providers to make changes to care delivery and payment that meet their priorities.
2. Integrating behavioral health into primary care. Behavioral health integration is an integral part of advanced primary care and a key feature of the Common Purchasing Agreement mentioned above. Nearly seven in 10 patients in need of behavioral health treatment seek care via primary care practices. Evidence shows that integrating behavioral health services into primary care can enhance mental health care access and coordination, improve outcomes and reduce costs. Behavioral health integration, a feature of advanced primary care, allows patients to access mental health care screening, services and treatments through their primary care provider, just like any other specialty care. Employers are highly focused on these efforts, which address an issue that has reached crisis level in this country.
3. Requiring members to choose a primary care provider. Patients benefit from an ongoing primary care relationship with improved care access, greater care continuity and better health outcomes. This in turn reduces employee absenteeism, enhances productivity and lowers overall health care spending for employers. That’s why some employers are taking additional steps to ensure their members are connected to a primary care practice. Methods to do so include mandating that members select a primary care physician and/or team, using benefit design incentives to support the use of primary care over specialty care (when appropriate) and increase education about the importance of having a primary care provider.
4. Helping employees identify and use only the highest quality primary care providers. Using quality measures, such as the PBGH advanced primary care measure set, purchasers and health plans can identify high-performing provider practices. Once those practices have been identified, employers can drive plan members to providers able to demonstrate that they provide high-value care, or the providers identified can be rewarded for their superior performance.
Employers understand better than anyone that the quality of health care their employees can access has a profound impact on their work, lives and productivity. The last few years working through the unprecedented challenges brought about by the pandemic have only reinforced the importance of continuing to strive to reduce disparities in health care and increase access to high-quality and more affordable services.
The same principles of aligning payment incentives and employer voices in primary care provides a model for other care verticals, including maternity care, oncology and musculoskeletal disorders, to name a few. Employers will increasingly work with organizations able to help design and implement the standards necessary to ensure they’re buying the best health care services available for the millions of employees, consumers and families throughout the nation who rely on their employers for health benefits.
A Little Less Conversation, A Little More Action
November 18th, 2021
“We’ve talked long enough. It’s long past time to take action. Our goal is to foster meaningful, widespread change in health care within three years.” – Elizabeth Mitchell, CEO of PBGH
Large employers and health care purchasers have increasingly begun to take actionable steps to strengthen primary care, the critical precursor to a high-quality, cost-effective health care system.
Extensive research and pilot programs over multiple decades have repeatedly shown that a robust, integrated and accountable approach to primary care—characteristics collectively defined as advanced primary care—can significantly reduce overall health care costs while improving patient outcomes and experience.
Efforts by the nation’s largest employers to transform health care reached a major inflection point this fall when nearly 200 employers gathered with their health plans and health care provider partners from across the country at the PBGH Primary Care Payment Reform Summit. The event created a platform during which employers collectively conveyed their readiness to implement tools designed to induce payers and providers to deliver the same levels of value and quality they routinely expect from other vendors, and their commitment to investing in advanced primary care with integrated behavioral health and a commitment to equity.
Here are 5 key takeaways from the summit about what large employers and purchasers want from their health care vendors:
1. Employers have long accepted poor value for their health care dollars in ways they never would for any other product or service.
Employer-sponsored health plans routinely pay 200-600% times the rates charged to Medicare and effectively provide most of the profit margin for both health plans and providers without visibility into the quality of care their employees receive. Years of provider and insurer consolidation means even the largest employers tend to lack enough employees in any market to exercise adequate leverage to compel greater transparency and accountability.
2. Purchasers feel they’ve given health care stakeholders ample opportunity to reform the care payment and delivery system.
Industry efforts to transform health care have largely failed due to a lack of shared alignment and goals, a fragmented care system, the continued reliance on fee-for-service and the industry’s resistance to change. Now purchasers are collectively taking action to improve value and quality. Read more about what purchasers are doing right now in the full report.
3. Point solutions are making fragmentation worse and threaten to further increase costs.
To better serve members and reduce costs, many employers are turning to third-party vendors for singular, or point, solutions that address specific care functions or services. While many of these new, often digital capabilities are useful in isolation, they’re collectively making worse the already substantial problem of fragmentation and complexity across the care continuum. Many are also backed by venture capital firms seeking maximum profit potential and hence have little incentive to reduce the overall cost of care.
4. Integrating behavioral health into primary care is vital.
Mental health has been a top priority for employers for many years, and the urgency has only increased during the pandemic. Mental health care is hard to access and of variable quality, but mental health care is primary care and needs to be part of advanced primary care practice. Evidence shows that integrating behavioral health services into primary care can enhance mental health care access and coordination, improve outcomes and reduce overall costs.
5. Achieving lasting change will require that purchasers pull together to achieve critical mass.
Employers today have an opportunity to leverage their immense buying power to promote fundamental change in how health care is accessed, purchased and delivered. But even the biggest purchasers in the country lack leverage in most markets. Change on this scale cannot occur unless purchasers work in concert in every region in the country. Only by collectively setting high standards and demanding change can employers hope to overcome the existing system’s enormous inertia.
The Time to Act is Now
Employers want to buy the best health care benefits on behalf of their employees. But they understand better than most how costly and dysfunctional our health care system has become. They provide the critical lifeline of health insurance to about half of Americans, and they grapple every day with ways to keep coverage affordable.
Read the full report A Little Less Conversation, A Little More Action: 5 Takeaways from the PBGH Primary Care Payment Reform Summit here.
See more about the PBGH Primary Care Payment Reform Summit here.
How Primary Care Providers Can Improve Depression Screening
May 4th, 2021
Depression screening is an essential tool for primary care providers to better understand and meet their patients’ needs, especially as behavioral health conditions have dramatically increased in the past year. Patient-centric approaches and thoughtful implementation of depression screening can lead to earlier intervention, improved overall health outcomes and reduced utilization of health care services.
In March 2021, PBGH’s California Quality Collaborative (CQC) hosted a webinar on the importance of depression screening for patients, providers and payers and shared practical advice for patient-centered depression screening. Experts from PBGH, Montefiore Medical Center and UCLA identified four key takeaways during the discussion:
1. Primary care providers should start screening patients for depression now. There is increasing demand being placed on primary care clinicians to screen patients for depression. Health plans, employers and other purchasers of health care recognize that depression affects millions of patients, and they are investing in behavioral health as a strategy to improve health outcomes. In California, there is momentum from organizations like the Integrated Healthcare Association, which runs statewide performance improvement programs, and Covered California, to include depression screening as a required health care quality measure. Providers will be financially accountable for completing depression screening in the next several years as part of existing pay-for-performance programs.
2. Care teams need training to be comfortable screening patients for depression. Care teams require resources and information about depression screening and how to follow up appropriately with patients in need of behavioral health services. Specialized trainings with role-playing opportunities are effective, as are resources, such as a list of frequently asked questions developed by the Advancing Integrated Mental Health Solution (AIMS) Center from University of Washington.
3. Screening workflows can be integrated into virtual visits, with intentional planning. During the public health emergency, UCLA Health increased the use of virtual primary care visits. The system’s clinical and operations teams created a depression screening workflow that leveraged “virtual rooming” steps, during which clinical support staff register and prepare patients for telehealth visits just as they would for in-person clinical appointments. To address safety concerns associated with suicidal ideation documented in patient depression questionnaires, they tested and implemented several solutions by which the provider would monitor a patient’s response, or the electronic health record would issue an automatic alert.
4. Technology can expand the reach of primary care to provide whole-person care. Montefiore Medical Center launched a smartphone app that includes screening, educational resources, appointment and medication reminders and near real-time chat, among other features. Providers using the Montefiore app with their patients found that it improved behavioral health care engagement with a diverse set of patient populations. In an analysis of the smartphone app pilot data, 72% of patients used it to access educational articles and videos, 69% used it to interact with their care teams via secure chat or text and 67% used the app to complete a depression or other behavioral screening scale.
For additional insights about how primary care providers can improve depression screening for their patients, watch the March 31 CQC webinar or access the presentation.
The Current State of Mental Health Screening and Access in California: Results from 35,000 Patients
October 26th, 2020
Mental health concerns are increasingly common, yet many patients in California are not screened for symptoms and are unable to access treatment. Understanding patients’ access to care is challenging; data are scarce and usually only available at a statewide level, even though there are likely wide regional differences due to workforce shortages.
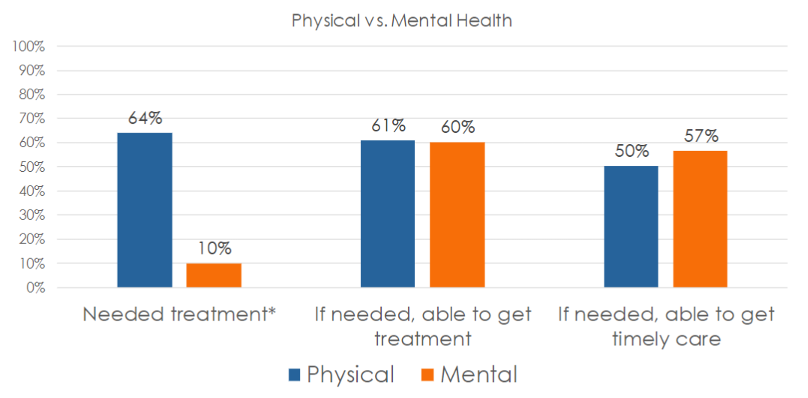
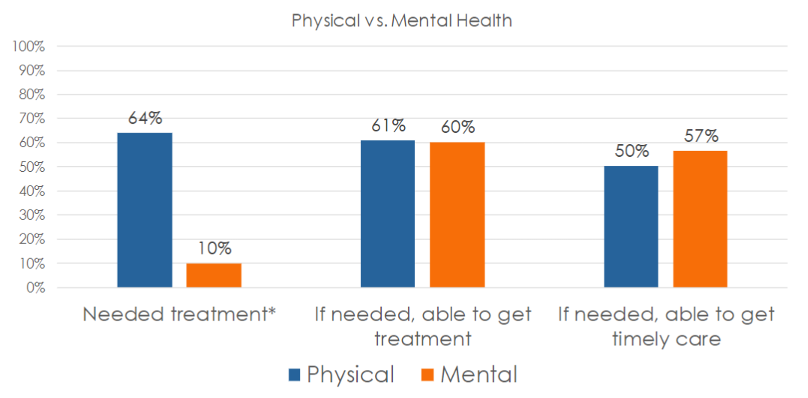
In its Accelerating Integrated Care webinar series , the Pacific Business Group on Health’s (PBGH) California Quality Collaborative presented results from the most recent PBGH Patient Assessment Survey (PAS). The research measured the experience of 35,000 Californians regarding mental health screening and access to necessary treatment. Also measured was the degree to which patients were successful getting timely access to physical versus mental health care.
Screening Rates and Access to Mental Health Treatment are Low
Participants of the survey visited either a primary care or specialty medical provider between July and October of 2019 and were asked to rate their experiences with their medical care during the six months prior to receiving the survey. Survey participants were asked a series of questions, including:
- Were you asked about mental health symptoms during your medical visit during the past six months?
- Was treatment recommended?
- Did you need treatment?
- Were you able to get care?
- Were you able to get care when you needed it?
Many patients (67%) said that no one from their provider’s office – whether a primary care or specialist visit — had asked them about their mental health, despite 16% reporting feeling they needed care and 30% having accessed care on their own. One-third (33%) said a provider asked them about their mental health.
Half of all patients who were screened were recommended for mental health treatment. Two-thirds agreed they needed the care that was recommended.

Whether in need of mental or physical health care, 60% of those surveyed said they were always able to get access to needed services. Surprisingly, a higher percentage of survey participants in need of mental health services (57%) said they were able to get care when they needed it, compared to just 50% seeking physical health services.
Using Patient Reported Data to Improve Access to Mental Health Care
All provider organizations can utilize this data to improve upon the rate at which patients are screened for mental health symptoms and to ensure they gain access to needed care. Using either baseline data or the Patient Assessment Survey data presented here as a proxy, comparisons against state benchmarks to set goals for screening and access can be made. To begin improvement work, select evidence-based change tactics to create an action plan.
It is important to ask patients about their experiences accessing care at your organization. Encounter and claims data can be useful in instances when patients who have been seen for a medical appointment have also filled out a screening tool, though this data do not capture whether the patient was satisfied with their experience and felt they received care when they needed it. Follow the steps below to capture feedback from patients to identify populations that might need extra support.
If your organization does not already collect such data:
- Measure: Develop a survey to collect patient data.
- Interpret: Use the data presented in this article as a proxy benchmark until you collect your own data – assume your screening and access rates are similar (33% screened, 60% able to access care).
If your organization already collects patient experience data for mental health care:
- Measure: Identify a contact at your organization who can provide data on mental health screening and access.
- Interpret: Compare your internal data to the statewide data presented in this webinar (33% screened, 60% able to access care) – how does your organization compare? Which populations might need extra support?
For more details on upcoming CQC webinars focusing on how to improve mental health screenings and access to mental health treatment in primary care settings, sign up for the CQC Newsletter or visit the Webinars webpage . Later this year, PBGH will publish an Issue Brief with further results from this study. For more information, find the full recording of this webinar here and the slide deck here.